Killer breast Cancer It’s on the rise among young women – and among people under 40 years of age, it’s been rising the fastest for more than two decades.
New diagnoses of metastatic breast cancer — when the disease has spread from the original site — among 20- to 39-year-old patients rose nearly three percent from 2004 to 2021, with a 1.4 percent increase among women in their 70s.
Radiologists affiliated with the American College of Radiology analyzed cancer diagnoses from 2004 to 2021, focusing primarily on women with aggressive breast cancer that had spread to other parts of their bodies.
Breast cancer starts in a specific place in a woman’s breast, but it can spread to other parts of the body, which greatly reduces the chances. The patient lives.
When breast cancer is detected early — before it reaches its peak — through preventive screening measures like mammograms, the five-year survival rate is high — 86 to 99 percent. However, once the cancer cells have migrated, the survival rate drops to just 31 percent.
Although cancer is traditionally seen as a disease of the elderly — more than 60 percent of cancers are diagnosed in people over 65 — U.S. health officials are recognizing the seriousness of the problem. Young adults are being investigated With the disease – usually the most advanced cases.
Experts say this growth is partly due to current screening guidelines not recommending mammograms until age 40, as well as delays in diagnosis and treatment. covid 19 Epidemic.
The researchers called their findings ‘exciting’ and warned that the current statistics may be an underestimate. In terms of the effects of the epidemic On monitoring and investigations.

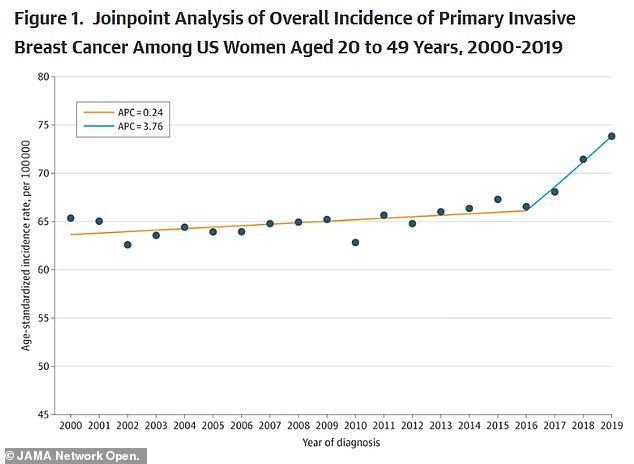
According to a recent study by JAMA, between 2000 and 2019, breast cancer increased by 0.79 percent annually. But after 2016, the increase became sharper
While Research The rate of metastatic breast cancer was significantly higher in young women than in older women, with similar rates in middle-aged women.
In the year From 2004 to 2012, cases in 40 to 74 patients increased two percent per year, and from 2018 to 2021, there is a 2.7 percent increase per year.
In the year By 2024, an estimated 311,000 women will be diagnosed with breast cancer and more than 42,000 will die.
About 80 million women’s records are included annually.
Dr Debra Monticciolo, co-author and past president of the American College of Radiology, said: ‘It is important to understand that these women have distant (metastatic or stage 4) breast cancer at diagnosis.
‘Women diagnosed with this disease have a very low survival rate and are very difficult to treat.’
Women under 40 are 39 percent more likely to die from the disease than those 40 and older.
They also tend to diagnose biologically more aggressive breast cancers, such as triple-negative breast cancer and HER2-positive breast cancer.
In 2009 Report In the year About 22,000 women aged 20 to 69 were diagnosed with invasive breast cancer between 1992 and 2005, and the youngest women (20 to 34) were less likely to survive the cancer in the next five years.

The researchers attributed the increase to gaps in screening, and young women are generally not recommended to get mammograms until their 40s, unless they know they have a genetic risk.
Compared to older women, they had the highest risk of dying, with the risk being three times higher.
As women get older, their risk of dying from breast cancer decreases.
For women aged 35 to 39, the risk is 1.76 times higher, and for those aged 40 to 49, the risk is only 1.17 times.
They also tend to diagnose biologically more aggressive breast cancers, such as triple-negative breast cancer and HER2-positive breast cancer.
Additionally, mutations in the BRCA1 or BRCA2 genes, which increase cancer risk by up to 84 percent, are more common. In young women. About 6 percent of women with breast cancer carry a BRCA gene mutation, but the number is closer to 12 percent of breast cancer patients under the age of 45.
This may be because, because BRCA affects early-stage cancers, mutations are more common in younger people, but cancers in older people can often be attributed to other factors, including hormonal, lifestyle or environmental factors.
Researchers have also suggested that isolation and quarantine measures during the outbreak may have prevented people from seeing their doctors for routine check-ups and preventive services such as mammograms in late-stage screenings.
In the year In 2020 and 2021, millions of people were afraid to leave their homes for fear of getting sick or couldn’t get in to see their doctors because they were thin with patients or working remotely.
Current screening protocols may also be a factor.
Federal mammogram guidelines recommend screening for women age 40 and older, if they don’t have a family history of the disease, but many women may be unaware of their risk, or may falsely believe that breast cancer affects only women of a certain age.

Maria Costa (seen here during treatment), 35, was diagnosed with stage three breast cancer a year after requesting a mammogram. She now fears that she will never be able to date or have children.

Nurse Holly McCabe, 31, always tells her patients about the importance of breast self-exams, but she didn’t do her own until August 2023.

In September, Ms McCabe began a regimen that included 16 rounds of chemotherapy, followed by a second round lasting 12 weeks.
And sometimes doctors can fall into the same delusion and not recommend testing to young women, even though those women are rightly concerned.
This happened in the case of 33-year-old Maria Costa. In 2022, she was diagnosed with invasive stage 3 breast cancer, one year after she requested a mammogram.
Although she has a family history of breast cancer – her mother and aunt were diagnosed – her gynecologist dismissed her concerns and told her she was too young after she felt a lump in her breast.
In the year It wasn’t until 2022 that she finally got a mammogram and was diagnosed with stage 3 invasive lobular carcinoma, a rare, slow-growing breast cancer that starts in the milk-producing glands.
This type of cancer accounts for 10 percent of breast cancers.
In the early stages, invasive lobular carcinoma has a survival rate of almost 100 percent, but this drops to 22 percent if it has spread.
Now 35, Ms Costa said she had to fight for doctors to take her seriously and believes her experience could be different if she was diagnosed in 2021.
Following her diagnosis, Ms. Costa went into medically induced menopause to reduce estrogen levels, which can fuel cancer growth.
Doctors stress young women’s anxiety about possible side effects of prescription birth control.

Sarah Citron, 33, was diagnosed with breast cancer earlier this year after noticing a lump on her armpit. Doctors first thought the boil was due to hormonal changes and removed the IUD to try another child

Actress Olivia Munn was diagnosed with breast cancer at the age of 42 and underwent a double mastectomy.
Sara Citron, 33, of California, was told that the first lump in her armpit after she had her birth control IUD removed could be due to hormonal changes.
She wasn’t overly concerned at first because she had a history of a cyst on her breast and believed the lump could be related to the recently removed or recent covid booster vaccine.
Her doctors assured her that breast cancer was highly unlikely due to her young age and suggested that she monitor the lump.
But, after the lump didn’t go away, Ms. Citron pushed for more tests, eventually persuading her doctor to do a mammogram last year. An examination revealed a mass, which was later confirmed to be cancerous on biopsy and had spread to her lymph nodes.
and Holly McCabe, a 31-year-old nurse from Denver, Colorado. She was diagnosed with stage 3 triple-negative breast cancer In the year After her first breast self-examination in September 2023.
As a nurse working in the oncology department at St. Joseph’s Medical Center, McCabe encourages her patients to get regular breast self-exams, but she never did one herself until August 2023.

Roisin Phelan, seen with her husband Michael, was diagnosed with breast cancer and given just three years to live.
Her decision to examine her breasts was sparked when she saw a patient at work finishing chemotherapy, an event that prompted her to examine her own health. During a self-examination, McCabe discovered a firm lump in her right breast.
Although she was young, healthy and had no family history of breast cancer, McBee underwent a series of self-diagnoses, which confirmed she had stage 3 triple-negative breast cancer.
Her story and others like it highlight the importance of screening and breast self-examination, regardless of age or family history, as a critical tool for early detection.
Dr Debra Monticciolo, a radiologist at the University of Colorado and co-author of the current report, said: ‘Our research shows that we are missing opportunities to detect disease early.
We’re losing it, and we really need to get women to check it out. We need to make women, radiologists and clinicians aware that these trends are unacceptable and must be reversed if we want to save women’s lives.’